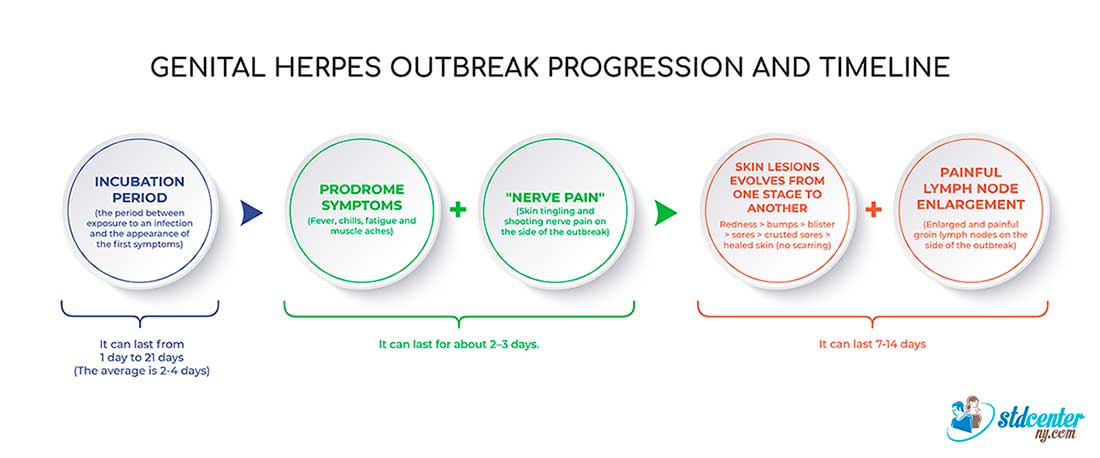
What is the herpes timeline?
This illustration summarizes the progression of the herpes outbreak and its timeline.
What are the stages of genital herpes, or how do herpes symptoms progress?
Each herpes outbreak consists of multiple stages.
Stage 1:
A symptomatic patient begins to experience a tingling or itching sensation in the area of exposure 12–24 hours after initial herpes exposure. In addition, systemic symptoms such as fever, fatigue, and headache might occur.
Stage 2:
Herpes-specific blisters develop in the affected areas. There are multiple blisters clustered on a red base.
Blisters almost always appear after stage 1 in symptomatic patients.
Occasionally, symptoms don’t progress to signs because the immune system acts fast, suppressing the outbreak, or because the person takes herpes-suppressive medication. This usually happens with flare-ups: the virus reaches the surface, and the skin becomes infectious, but no signs of herpes appear.
The first outbreak can take 2–12 days (the average is four) before lesions appear; in subsequent outbreaks, skin blisters can occur as soon as 12 hours after stage 1.
Stage 3:
The blisters break within seven days of appearing and leave aching ulcers or sores (which may bleed).
Stage 4:
Once ulcers develop, healing takes about 1–4 weeks. Scars don’t develop. The time is longer (2–4 weeks) for newly infected people and shorter (1 week) for people experiencing a recurrence.
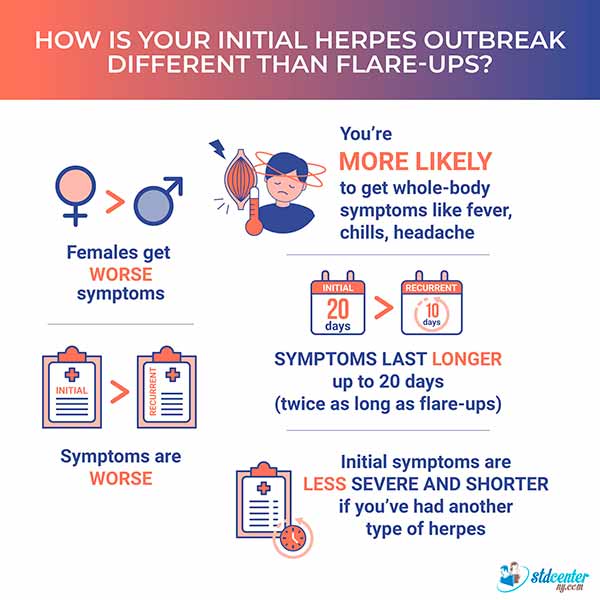
First herpes outbreak
The symptoms of a first herpes outbreak are more severe and last longer than those of flare-ups. This is most likely because the immune system reacts to an unfamiliar virus.
The average duration of symptoms for an untreated initial outbreak is 20 days. New skin lesions might continue to develop for the first 5–7 days.
Here are more important facts about the first outbreak:
✓ The initial outbreak tends to be more severe in females.
✓ The chance of getting systemic symptoms like fever, chills, and headache is much higher with the first outbreak.
✓ The symptoms are less severe and shorter in people with another type of herpes.
This picture summarizes how the first herpes outbreak differs from flare-ups.
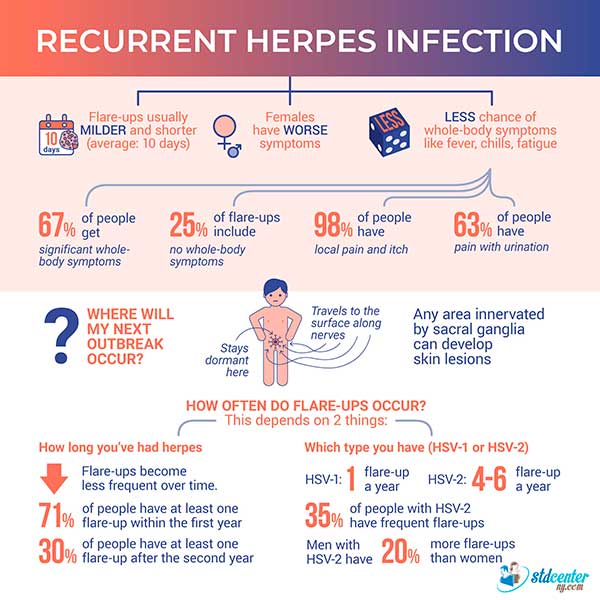
Recurrent herpes outbreak
Some patients might have one outbreak, and some might get recurrent outbreaks.
After the first outbreak, the herpes virus travels along nerves from the skin to the sacral ganglia (a bundle of nerves) in the spine and remains inactive for some time. Once activated, the virus can travel from the ganglia to the skin's surface, causing a flare-up.
A recurrent herpes outbreak is usually milder (the symptoms are less severe) and shorter than the first outbreak.
Where do recurrent herpes skin lesions appear?
Recurrent herpes skin symptoms might occur in the same anatomic area as the initial outbreak or close to it. Since the herpes virus stays dormant in the sacral ganglia and travels along nerves to the surface of the skin, any skin in the genital area innervated by the sacral ganglia (that is, any skin connected by nerves to the sacral ganglia) can undergo a flare-up. Therefore, it’s possible to have recurrent herpes outbreak in the anal area without ever having anal sex.
How often should I expect recurrent herpes outbreaks, and what are the main factors affecting that?
Flare-ups may occur frequently in some patients. It depends on how strong their immune system is, how long they’ve had herpes, and the type of herpes virus (HSV-1 or HSV-2) affecting the area.
How does the immune system affect the frequency of recurrent herpes outbreaks?
The stronger the immune system, the less likely a flare-up will occur. The immune system is weakened by illness, emotional stress, and certain medications.
How is the frequency of herpes flare-ups affected by disease duration?
Herpes is a regressive condition, which means the number of flare-ups and their severity decrease over time.
On average, about 71% of people will have at least one flare-up within the first year after the first outbreak. The number of people who have a flare-up drops to 30% after the second year.
The more severe the initial episode, the greater the chance of flare-ups, whether medication was taken or not.
The different herpes types HSV-1 and HSV-2 have different recurrence rates. Flare-ups of HSV-2 in the genital area occur more often than those of HSV-1.
Around 80% of people with HSV-2 have one flare-up after the first outbreak, while 50% of people with HSV-1 do. And 35% of people with HSV-2 have frequent flare-ups. Flare-ups of HSV-2 in the genital area occur more often than those of HSV-1.
Males with HSV-2 have about 20% more flare-ups than females—which explains the higher transmission rate from males to females.
How are recurrent herpes symptoms different?
Recurrent herpes outbreaks are shorter than the first outbreak, lasting an average of 10 days (if not treated).
Recurrent herpes symptoms are more severe in females than in males.
Here are some random statistics about recurrent herpes outbreaks that you may find interesting and helpful:
✓ 67% of people get significant systemic (whole-body) symptoms
✓ 25% of recurrent herpes episodes have no systemic symptoms
✓ 98% of people have local pain and itch
✓ 63% of people have pain with urination
This illustration summarizes the recurrent herpes infection.
Source
-
Genital herpes NHS
https://www.nhs.uk/conditions/genital-herpes/ -
Genital herpes: signs and symptoms
https://www.aad.org/public/diseases/a-z/genital-herpes-symptoms -
Human herpes simplex virus infections: epidemiology, pathogenesis, symptomatology, diagnosis, and management
https://pubmed.ncbi.nlm.nih.gov/17939933/ -
Chapter 1943. Herpes simplex. Access medicine
https://accessmedicine.mhmedical.com/content.aspx?bookid=392§ionid=41138922