What is oral sex?
Any contact involving the mouth, lips, and tongue to stimulate a partner's vagina (cunnilingus), penis (fellatio), or anus (anilingus) is categorized as oral sex. This also includes oral stimulation of the surrounding skin areas known as the peri genital and perianal regions.
STDs that can be transmitted through oral contact
- - Chlamydia
- - Gonorrhea
- - Herpes
- - Syphilis
- - HPV
- - HIV
The Risks of STDs From Oral Sex
This section discusses the risks of contracting STDs from oral sex, distinguishing between performing and receiving oral sex. The likelihood of acquiring STDs from receiving oral sex is generally lower than from performing it. Why is that? This is because the enzymes in saliva neutralize many viral particles, even in the presence of blood in the saliva.
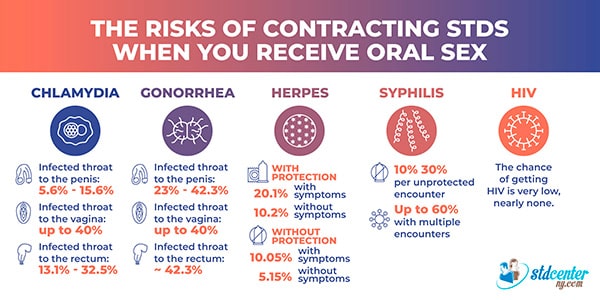
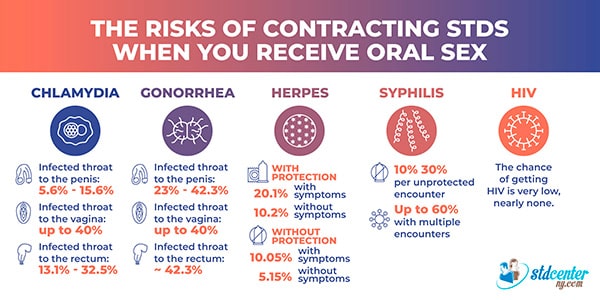
When you are Receiving Oral Sex
Chlamydia
- - Probability of transmission from an infected throat to the penis: 5.6% - 15.6%
- - Risk of spreading chlamydia from an infected throat to the vagina: up to 40%
- - Likelihood of transferring chlamydia from the infected throat to the rectum: 13.1% - 32.5%
Gonorrhea
- - Chance of transmission from an infected throat to the penis: 23% - 42.3%
- - Transmission rate from an infected throat to the vagina: up to 40%
- - Risk of transmission from the infected throat to the rectum: approximately 42.3%
Syphilis
The risk of transmitting syphilis through oral sex is estimated to be 10% - 30% per unprotected encounter, increasing to 60% with multiple unprotected encounters with the same partner.
Herpes
Transmission occurs at 20.1% when symptomatic and 10.2% when asymptomatic.
With protection (such as a condom or dental dam), the risk decreases to 10.05%with symptoms and 5.15% without symptoms.
HIV
The chance of getting HIV from oral sex with an HIV-positive person is very low, nearly none.
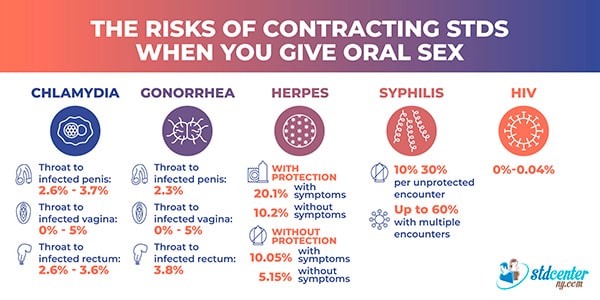
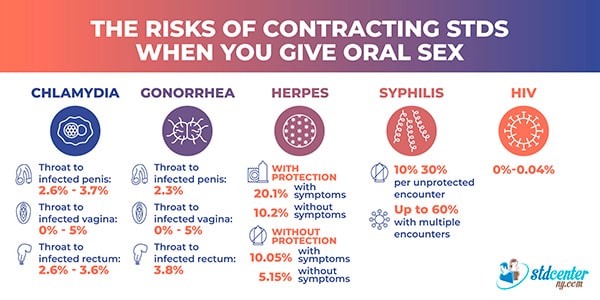
Giving Oral Sex
Chlamydia
- - Probability of transmission from an infected penis to the throat: 2.6% - 3.7%
- - Risk from an infected vagina to the throat: 0-5%
- - Likelihood of transferring chlamydia from the infected rectum to the throat: 2.6%-3.6%
Gonorrhea
- - Chance of transmission from an infected penis to the throat: 2.3%
- - Risk from an infected vagina to the throat: 0 - 5%
- - Risk from the infected rectum to the throat: 3.8%
Syphilis
The risk of syphilis transmission from giving oral sex is also estimated to be 10% - 30% per unprotected encounter, increasing to 60% with multiple unprotected encounters with the same partner.
Herpes
The transmission risk is 20.1% if symptomatic and 10.2%if asymptomatic. When protection is used, the likelihood decreases to 10.05% with symptoms and 5.15% without symptoms.
HIV
- - The risk of receiving oral sex from an HIV-positive person—whether involving the penis, or rectum—is very low, estimated at 1 in 2,500 acts (0%-0.04%)
- - There is no chance of contracting HIV through cunnilingus, as no documented cases of this have been reported in reliable sources.
What Factors Influence STD Spread During Oral Sex?
The likelihood of contracting an STD during oral sex, as well as the risk of transmission to others, is influenced by several factors:
Role in the Encounter:
Are you the one receiving or giving oral sex? Generally, performing oral sex carries a higher risk of contracting STDs.
Frequency of Sexual Acts:
Having oral sex more often raises the likelihood of transmission.
Duration of the Act:
The longer the sexual act lasts, the higher the likelihood of STD transmission.
Types of STDs that you can contract.
Some STDs spread more easily than others.
FAQs
Oral Sex vs. Vaginal or Anal Sex: Which is Safer? ›
What is the likelihood of contracting and transmitting gonorrhea through mouth-to-mouth contact (deep kissing)? ›
Is the risk of contracting chlamydia and gonorrhea from receiving oral sex different for homosexuals and heterosexuals? ›
Why is the chance of contracting HIV with oral sex so low? ›
What must I know about the oral transmission of the two herpes types without symptoms? ›
Source
-
About STI Risk and Oral Sex
https://www.cdc.gov/sti/about/about-sti-risk-and-oral-sex.html -
Sexually Transmitted Infections
https://www.ncbi.nlm.nih.gov/books/NBK560808/ -
Oral sex and transmission of non-viral STIs
https://pubmed.ncbi.nlm.nih.gov/9634339/ -
Sexually transmitted infections in oral cavity lesions: Human papillomavirus, Chlamydia trachomatis, and Herpes simplex virus
https://pmc.ncbi.nlm.nih.gov/articles/PMC6598522/