What is avaginal sore?
A vaginal sore (also called an ulcer) is a small,slow-healing wound on the vaginal surface. It forms when a virus, bacteria, trauma (cut), or allergen irritatessensitive vaginal tissue. The body responds by releasing special cells that worsen the irritation. One or more sores develop. Once the sore has developed, the ongoing bacterial exposure in the area makes it difficult for it to heal.
Causes of vaginal sores
Vaginal sores can be caused by STDs and non-STDs.
Here we will list the most common causes of vaginal ulcer in general.
STD causes of genital sores
- Herpes
- Syphilis
- Granuloma inguinale
- Molluscum
- Chancroid
- Genital warts
Infectious causes of vaginal sores that are not STDs
- Advanced yeast infection
- Epstein-Barr virus
- Cytomegalovirus (CMV)
- Varicella zoster virus
- Group A strep
Other causes of vaginal sores
- Valvular aphthae
- Vaginal cut or friction burn
- Contact dermatitis
- Trauma or infected scratch
- Cyst or Bartholin abscess
- Hidradenitis suppurative
- Vulvar cancer
STDs that cause vaginal sores
Several STIs(sexually transmitted infections) can lead to open sores of the vagina. These conditions can be transmitted via oral sex, vaginal sex, or anal sex.
So, what does a vaginal ulcer(sore) caused by an STD look like?
Here we will describe vaginal sores caused by various STDs.
In addition to giving a description and providing pictures, we will list other common symptoms associated with the condition, say what its incubation period is, and provide testing and treatment overviews.
Herpes sore
Both herpes virus types (HSV-1 and HSV-2) can cause vaginal (or vulvar) sores. They are transmitted through skin-to-skin contact. When symptoms are present, there is a 20% chance of passing the infection. When no symptoms are present, there is a 10% chance of passing it (during "silent shedding").
HSV-2 is a more common cause of genital sores than HSV-1 is.
HSV-2, or "genital herpes," is more common among females than males (15.9% versus 8.2%). This is probably because it is more easily transmitted by men to woman due to the female genital anatomy(the vagina has a bigger mucosal area than the penis).
The incubation period is 2-12 days after exposure, with an average of 4 days. Not every infected person becomes symptomatic-only 10%-25% develop symptoms.
In symptomatic people, the earliest symptom is an itch and burning sensation of the skin, which turns into a bump, which eventually transforms into blisters. The roofs of the blisters come off, forming sores. Over a few days, scabs form over the sores and they heal without leaving scars.
A herpes outbreak can have other nonspecific systemic symptoms, such as fever, chills, fatigue and flu-like symptoms.Lymph nodes locally (on the side of the sores) become enlarged and painful.
What does a herpes vaginal sore look like?
Herpes vaginal sores are very superficial. They affect the top layer of the vaginal mucosa and do not penetrate deep into the vaginal tissue. The fact that the sore is superficial can be appreciated visually (by an experienced doctor) or can be confirmed by a pinch test.
The area with herpes sores, when pinched with the fingers, does not feel thicker than the normal adjacent area.
In addition to being superficial (which is the most important characteristic), herpes lesions are multiple and clustered.Transparent fluid can be seen when the roof of the blister comes off.
Syphilis
Syphilis vaginal (or vulvar) sores are caused by bacteria called Treponema pallidum.
The bacteria get under the broken skin via skin-to-skin contact.
Syphilis is more common in men than women. In 2015, of the almost 24,000 people in the United States diagnosed with syphilis, only around 2,200 were women.
The incubation period (time from acquisition to developing symptoms) for syphilis is 10-90 days, with an average of 21 days.
In addition to skin symptoms, syphilis (depending on the disease stage) can cause sore throat, fever, muscle ache, fatigue, and lymph node enlargement.
What does the syphilis vaginal sore look like?
A syphilis sore is usually solitary (single) and round, with firm borders (hard borders felt when touched) and a clean base (you can see "raw meat" at the bottom of the sore and no pus at the base of the sore). A syphilis sore is painless (and this is a very important characteristic).
The sore will take 3 to 6 weeks to heal with or without treatment.
Chancroid
A vaginal/vulvar ulcer due to chancroid is caused by the bacterium Haemophilusducreyi.
The incubation period is 4-10 days after exposure.
Chancroid is not common in the United States. It is more common in Asia, Africa, and the Caribbean.
The disease presents with fever, chills, multiple lesions, and locally enlarged lymph nodes.
What does the chancroid vaginal sore look like?
Chancroid presents as multiple painful sores that are soft to the touch (unlike syphilis).
Granuloma inguinale
Vaginal granuloma inguinale (or donovanosis) is caused by the bacterium Klebsiella granulomatis.It is not common in the United States but is widespread in India, South Africa, and South America.
The incubation period (time from acquisition to developing symptoms) is 8-80 days.
The disease starts with one or multiple painless bumps that get larger and eventually ulcerate. The ulcer can easily bleed and might be smelly. Lymph nodes are usually not enlarged.
What does the granuloma inguinale vaginal sore look like?
This is a painless sore that slowly get bigger. There is no regional lymph node enlargement. The most important characteristic of the granuloma inguinale sore is that it easily bleeds due to its vascularity (i.e., it contains blood vessels).



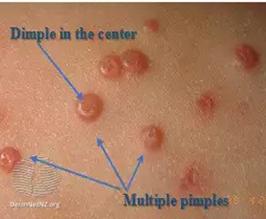
Molluscum contagiosum
Molluscum contagiosum is caused by pox family virus. There are two ways of getting an infection: direct contact with infected skin or contact with an object that has the virus on it.
The incubation period is from 1 week to 6 months (average of 2-3 months).
Molluscum results only in skin symptoms-small skin-colored bumps with a small dent at the top near the center. The bumps can be mildly itchy. This condition has no systemic symptoms.
What doesthe molluscum vaginal sore look like?
The molluscum sore forms from a bump. The sore is formed when the roof of the bump comes off.
The bumps are small, raised, and flesh-colored, with a dimple in the center.
Common non-STDs that cause vaginal sores
Vulvar aphthae
Vulvar aphthae are believed to be caused by immune system overreaction and are often precipitated by a viral syndrome. They are often preceded by sore throat and low-grade fever. They are most common in girls aged 9 to 18 years.
Genital aphthae are usually much larger than oral aphthae (cancer sores).
They are often mistaken for a STD.
What do vulvar aphthae look like?
The aphtha sore is large and deep, has well-defined borders, and is soft to the touch. The bottom (or base) of the valvular aphthae (similar to oral aphthae, or cancer sores) can be yellowish. It is very painful to the touch (unlike herpes sores,which hurt all the time).


Vaginal cuts or wounds
Vaginal or vulvar wounds can occur for various reasons, including the following:
- friction during sex
- allergy to fabrics or pads
- pubic hair removal
Like any cut on the body, a vaginal cut can becomeinfected.
What does a vaginal/vulvar cut look like?
A vaginal or vulvar cut is a prolonged wound that can be of different sizes and depths. There is minimal swelling and redness around the cut. There might be yellowish discoloration at the base due to a superimposed bacterial infection.
Advanced yeast infection
Vaginal yeast infection (also known as candidiasis) is a fungal infection caused by overgrowth and penetration of the fungus into deep vaginal cell layers.It affects 3 of 4 women at some point in their lifetime.
What do advanced yeast infection sores look like?
The entire area (vulva and vagina) is irritated, with significant redness, swelling,and small, superficial cracks and sores. White "cottage cheese" vaginal discharge is usually present.
Bartholin abscess, or cyst
The Bartholin glands are located on each side of the vaginal opening. They secrete fluid for vaginal lubrication. Occasionally, they can get obstructed, causing the fluid to back up and form a Bartholin cyst(which is usually painless). The fluid inside the cyst might get infected, causing a painful abscess. When the content of the abscess-pus-comes out,a sore is formed.
Hidradenitis suppurativa
Hidradenitis suppurative is a painful, chronic skin condition caused by inflammation and infection of the sweat glands. It usually occurs near the hair follicles.

Contact dermatitis
Contact dermatitis is a skin rash caused by contact with allergens, such as soap, cosmetics, fragrance, or jewelry. If one of these things irritates the skin, it might induce an allergic reaction.
The main symptomsare redness, swelling, and severe itch.
What does female genital contact dermatitis look like?
Pay attention to bilateral, symmetric, redness and swelling of the area. A vaginal and vulvar sore can be caused by allergens and secondary scratching.
What tests are used to diagnose vulvar ulcers?
Since female genital sores have many causes, a thorough evaluation is important. Agenital sore evaluation consists of three parts:
History of the sore
The healthcare provider will ask questions to learn more about the sore: how it appeared, if its appearance is changing over time, what symptoms preceded its appearance, and any other symptoms, such as fever, chills, and flu-like symptoms.What activity preceded the sore's appearance and the patient's sexual history are important as well.
Physical examination of the sore
A physician will check the sore and adjacent skin. The doctor may also examine other areas of the pelvis and feel for enlargement of lymph nodes.
Lab test
A lab test may be necessary to determine the cause of the ulcer.
- Blood test to check for herpes, EBV, CMV, RPR (syphilis)
- Swab test to check for herpes (can be done only if the sore is fresh), yeast infection, varicella, chlamydia, and gonorrhea
- Biopsy might be necessary if the ulcer is nonhealing and the cause cannot be determined by other methods
- Blood test to check for CRP, ESR, and ANA might be necessary; these are nonspecific inflammatory markers that help with the diagnosis of inflammatory conditions, such as Behcet's disease
- Pap smear to check forHPV
In a sexually active female, STDs need to be excluded first.
Home treatment of vaginal sores
Certain things can be done to relieve symptomsof vaginal sores (pain, itchiness, redness) while the patient is waiting to be diagnosed:
- Topical (xylocaine viscous) or oral (ibuprofen) painkiller
- Cool compress for swelling and redness
- Warm compress for pain and itchiness
- Sitz bath with warm water for about 15-30 minutes.
- Maintain clean genital area by washing the vagina with gentle saline water or baking soda
Ideally, see a healthcare provider before treating yourself. Any treatment that changes the initial appearance of the sore can make it harder for the doctor to establish the correct diagnosis.
Prescription medication treatment for vaginal sores
Once the diagnosis is established, disease-specific medication is prescribed based on the CDC's(www.cdc.gov) recommendations:
- Herpes (HSV-1 orHSV-2) is treated with antiviral medication: valtrex or acyclovir
- Syphilis is treated with a long-acting penicillin shot
- Chancroid can be treated with oral antibiotics: azithromycin, cipro, or erythromycin
- Granuloma inguinale or donovanosis is treated with azithromycin taken for 3 weeks
- Molluscum contagiosum is treated with cryotherapy or Aldara cream
- Yeast infection is treated with Diflucan
- Valvular aphthae are treated with 2% lidocaine gel
- Contact dermatitis or skin allergic reaction is treated with topical steroid cream
- Bartholin abscess is treated with an oral antibiotic or surgical drainage
- Hidradenitis suppurative is treated with an oral antibiotic and a topical steroid shot
When to see a doctor for vaginal sores
See a doctor if you:
- Find any unexplained genital sore
- Think it might be an STI
- Have genital itch that does not go away with basic home care
- Have pelvic pain, fever, chills, vaginal bleeding, or any other symptoms in addition to vaginal sore
Vaginal sores are nothing to be ashamed about. They are extremely common, and your doctor is there to help you.